Please note that our research only involves adult human volunteers. It is our policy never to test on animals or human embryo’s.
Professor Jo Spencer
Jo Spencer has had a career-long interest in human immunology, in particular the structure and function of the gut-associated lymphoid tissue and the origin of human intestinal IgA plasma cells.
It has recently become evidence that intestinal immune system can shape many factors that regulate the entire systemic immune system and that failures in this system can lead to autoimmunity. Her current research in the Department of Immunobiology at Guy’s hospital focuses on the association between intestinal autoimmunity and autoimmunity, in particular systemic lupus erythematosus and granulomatosis with polyangiitis.
Professor Deena Gibbons
Professor Deena Gibbons has had a long interest in immunology, in particular the development and function of the immune system in human infants, how this impacts lifelong immunity and subsequently the development of different autoimmune diseases.
Deena currently works in the Department of Immunobiology at Guy’s hospital focusing on B cell phenotype in human infants and how this compares to B cells in systemic lupus erythematosus.
Dr Sahil Jain
Dr Sahil Jain - Post-CCT Senior Clinical Research Fellow, Louise Coote Lupus Unit, Guy’s Hospital. London.
Dr Jain qualified medical school in 2010 from Maulana Azad Medical College in New Delhi, India. Subsequently he completed his post-graduate training in Internal Medicine from India and dual accredited training in Rheumatology and General Internal Medicine from the West of Scotland deanery.
With his special interests in SLE and vasculitis, he relocated to London to work at the prestigious Louise Coote Lupus Unit at Guy’s Hospital.
He is currently working as a post-CCT Senior Clinical Research fellow, and is a sub-investigator for several trials in SLE and vasculitis. Under the tutelage of Professor Jo Spencer and Professor David D’Cruz, he is investigating the possibility that DNA from gut bacteria could drive the production of anti-DNA antibodies that are a key feature of disease in patients with lupus.
My World has shrunk
Dr Melanie Sloan from the University of Cambridge led a new study exploring impact of Systemic autoimmune rheumatic diseases (SARDs) on patients lives.
Systemic autoimmune rheumatic diseases (SARDs) can involve physical, cognitive and mental health symptoms which have widespread impacts on patients’ lives. This study aimed to explore how SARDs impact patients’ daily activities, work, relationships, wellbeing and identity.
Alana Dalton
Alana Dalton completed her BSc in Biomedical Science at the University of Sussex before specialising in Immunology with a Master's degree at King’s College London.
She subsequently began her PhD at King’s College London under the supervision of Professor Deena Gibbons and Professor Jo Spencer, funded by the Lupus Trust.
Now in the third year of her PhD, her research focuses on B cells in human infants, exploring their development and potential function during bacterial infections.
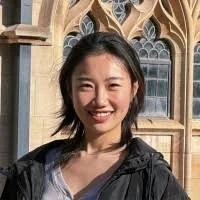
Xiaowen Sun
Xiaowen Sun achieved a Distinction grade in her Masters degree in Immunology at KCL, graduating in 2025. As part of this course, she did a research project in the Spencer lab where she learned computational methods for analysis of electronic image data.
She is now a Research Assistant funded by the Lupus Trust, studying cells in the human gut and liver tissues that we propose are responsible for identifying and breaking down DNA from gut microbes, to prevent microbial DNA from stimulating an anti-DNA response systemically.
Xiaowen is currently looking for a PhD studentship starting 2026 to support her ambition to become an independent scientist.
'I believe you' the words patients want to hear from doctors
A ‘chasm of misunderstanding and miscommunication’ is often experienced between clinicians and patients, leading to autoimmune diseases such as lupus and vasculitis being wrongly diagnosed as psychiatric or psychosomatic conditions, with a profound and lasting impact on patients, researchers have found.
A study involving over 3,000 participants – both patients and clinicians – found that these misdiagnoses (often termed “in your head” by patients) were often associated with long term impacts on patients’ physical and wellbeing and damaged trust in healthcare services.
Why nightmares and ‘daymares’ could be early warning signs of autoimmune disease
An increase in nightmares and hallucinations – or ‘daymares’ – could herald the onset of autoimmune diseases such as lupus, say an international team led by researchers at the University of Cambridge and King’s College London.
The researchers argue that there needs to be greater recognition that these types of mental health and neurological symptoms can act as an early warning sign that an individual is approaching a ‘flare’, where their disease worsens for a period.
Amaka Ejibe - Research Trial Coordinator.
Amaka studied a degree in Pharmaceutical Science at Kingston University and graduated in 2004.
She has been working in varying roles within Clinical Research since 2005 and working within Lupus Research since 2015.
Her role as a Clinical Trial Coordinator is to support Doctors, Pharmacy and Research Nurses facilitate Research within the department.
Time to move on from ‘doctor knows best’, say experts, as study finds clinicians rank patient views as least important in diagnosis
Experts today call for more value to be given to patients’ ‘lived experiences’ as a study of over 1,000 patients and clinicians found multiple examples of patient reports being under-valued.
The research, led by a team at the University of Cambridge and Kings’ College London, found that clinicians ranked patient self-assessments as least important in diagnostic decisions, and said that patients both over- and under-played their symptoms more often than patients reported doing so.
Study finds ‘startling’ levels of hidden mental health symptoms among autoimmune disease patients
Association between COVID-19 and the risk of developing Autoimmune conditions
Dietary changes may improve symptoms in patients with SLE
Drug combination could be new lupus treatment
Lupus clues from cellular 'power stations'
Researchers at Imperial College London have revealed crucial insights into systemic lupus erythematosus (SLE).
Previous studies from the same Imperial College researchers have suggested that immune cells called CD8 T cells, which normally help to destroy threats to the body such as viruses, appear to malfunction in SLE patients. This may play a role in the immune system spiralling out of control.
Vitamin D deficiency linked to metabolic changes in patients with lupus
Hydroxychloroquine ineffective against Covid-19
The role of the gut in the development of the immune system and how this is defective in SLE
Women 4 times more likely to develop Lupus after stillbirth
Women who suffer the tragedy of stillbirth are four times more likely to develop Lupus in later life than those who experience an uncomplicated birth, a study has found.
Researchers from Manchester found a link between stillbirths and connective tissue disorders — with the association with Lupus being by far the strongest.